Air You Can't See, Sleep You Can't Keep
Studies have consistently shown a strong link between exposure to fine particulate matter (PM2.5) and sleep disturbances. These tiny particles, with a diameter of less than 2.5 micrograms, are small enough to be inhaled deep into the lungs and even enter the bloodstream, causing a range of physiological and neurological effects that disrupt sleep.
How PM2.5 Affects Sleep
The impact of PM2.5 on sleep is multifaceted, affecting both the physical aspects of breathing and the body's natural sleep-wake cycle. Here are the key mechanisms:
- Respiratory Irritation
PM2.5 irritates the airways, worsening asthma and rhinitis, and causing coughing, wheezing, and shortness of breath that disrupt sleep. - Sleep Apnea
Air pollution increases the risk and severity of Obstructive Sleep Apnea (OSA) by narrowing airways, leading to frequent breathing interruptions and fragmented sleep. - Sleep Stage Disruption
Exposure to PM2.5 alters NREM and REM sleep and raises the arousal index, reducing sleep quality. - Systemic Effects
Once in the bloodstream, PM2.5 triggers inflammation and oxidative stress, affecting the brain and potentially causing neuroinflammation. - Circadian Rhythm
PM2.5 may disrupt the body’s natural sleep-wake cycle, contributing to insomnia and sleep loss.
Long-Term Health Consequences
Chronic exposure to PM2.5 and the resulting poor sleep quality can have serious long-term health consequences, including an increased risk of:
- Cardiovascular Disease:
Poor sleep quality and exposure to air pollution are both risk factors for heart disease. The combination can amplify this risk. - Cognitive Decline:
Sleep plays a vital role in memory consolidation and brain health. PM2.5 exposure and the resulting poor sleep have been linked to cognitive impairment and a greater risk of neurodegenerative diseases. - Mental Health Issues:
Poor sleep is a known risk factor for depression and anxiety. PM2.5 exposure can further exacerbate these issues.
Mitigating the Impact
To reduce the impact of PM2.5 on your sleep, consider the following measures:
- Keep Windows Closed:
On high-pollution days, keep your windows closed to prevent outdoor pollutants from entering your home. - Reduce Indoor Pollutants:
Avoid or limit sources of indoor air pollution, such as tobacco smoke, certain cleaning products, and scented candles. - Monitor Air Quality:
Pay attention to local air quality reports and limit outdoor activities on days with high pollution levels. - Improve Indoor Air Quality:
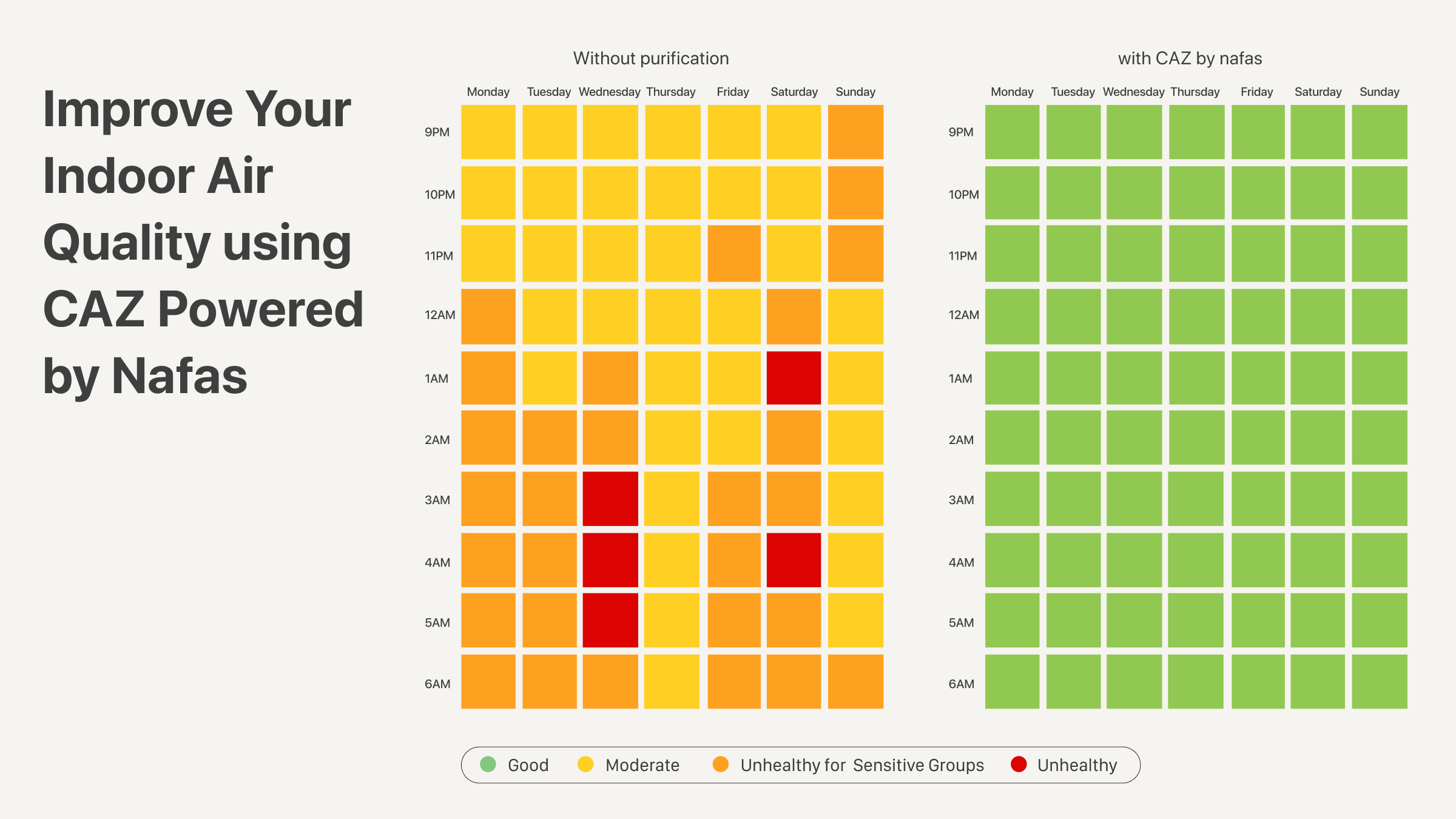
Looking at the chart above, the air quality during sleep time over the course of a week is noticeably different between a room without CAZ and one with CAZ by Nafas.
- Without CAZ, air quality tends to fluctuate. At certain hours of the night until early morning, the colors shift to yellow, orange, or even red. This indicates that the air falls into the categories of moderate, unhealthy for sensitive groups, and even unhealthy. Such conditions can definitely affect sleep quality and respiratory health.
- With CAZ, the results are much more stable. Throughout the entire week, the air quality during sleep time consistently stays green, which means good. This ensures the air we breathe while sleeping remains clean and healthy, without dangerous fluctuations.
With CAZ by Nafas, sleep becomes more restful because we can breathe air that maintains its quality all night long.
Source:
He, T., Cai, J., Duan, S., Liang, L., Liu, Y., Fu, W., Li, J., Zeng, X., & Chen, R. (2022). Early-Life Exposure to PM2.5 and Sleep Disturbances in Preschoolers from 551 Cities of China. American Journal of Respiratory and Critical Care Medicine, 207(5), 602–612. https://doi.org/10.1164/rccm.202204-0740OC
Lin, L., Liu, C., Chen, J., Li, Y., Su, T., Li, R., & Wu, C. (2025). Air pollution and sleep health in middle-aged and older adults: A systematic review and meta-analysis. Sleep Medicine. https://doi.org/10.1016/j.sleep.2025.07.032
Liu, M., Zhou, F., Li, C., Deng, X., & Liu, M. (2020). Effects of atmospheric particulate matter pollution on sleep disorders and sleep duration: A cross-sectional study in the UK biobank. Sleep Medicine, 74, 152. https://doi.org/10.1016/j.sleep.2020.07.032
Ramos, I., Silva, P., Pinho, J., & Lopes, S. (2022). Influence of indoor air quality on sleep quality of university students in Lisbon. Atmospheric Pollution Research, 13(11), 101569. https://doi.org/10.1016/j.apr.2022.101569
Xu, Y., Cai, Y., Liang, L., Li, X., Wang, X., Wang, X., & Shen, X. (2018). Association between long-term exposure to air pollution and sleep disorder in Chinese children: The Seven Northeastern Cities study. Sleep, 41(9), zsy123. https://doi.org/10.1093/sleep/zsy123